With the novel coronavirus continuing to spread across the nation, the impacts have been uneven, both in terms of who is more likely to be exposed to the virus, and in terms of who is most likely to experience serious complications. These high-risk groups include adults over 65 years of age, as well as people with severe underlying health conditions. According to data from the CDC’s Behavioral Risk Factor Surveillance System, almost one in four of D.C.’s adult residents have an increased risk of developing severe illness if they are infected by COVID-19, based on age or underlying health conditions.
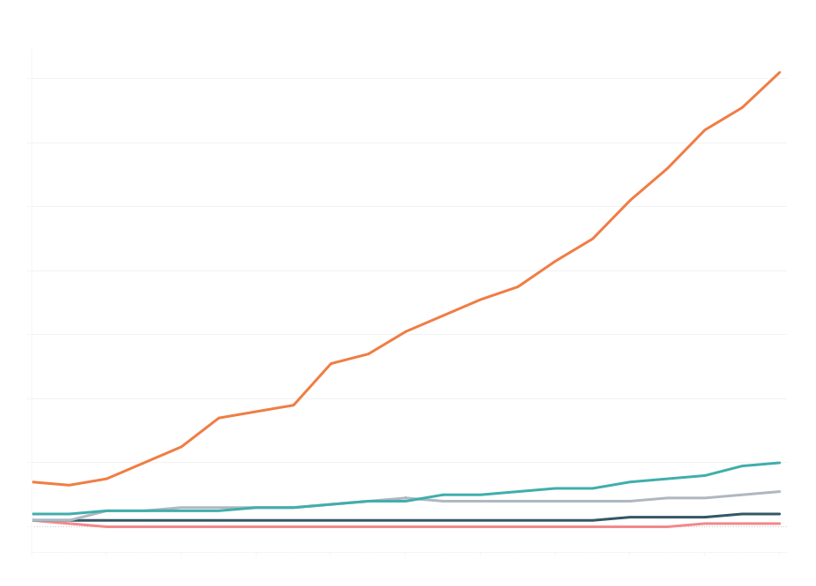
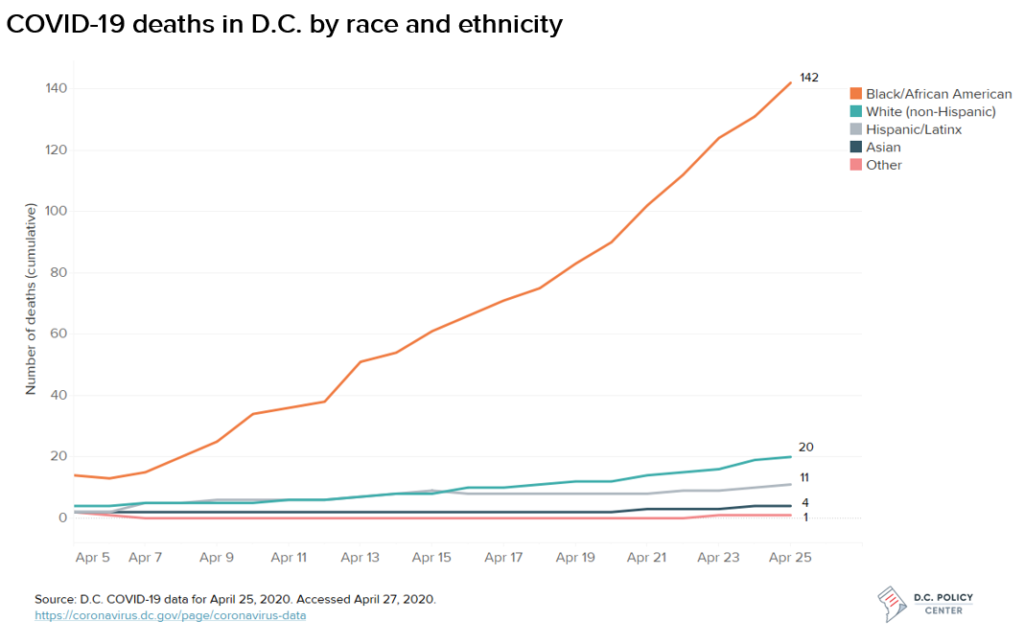
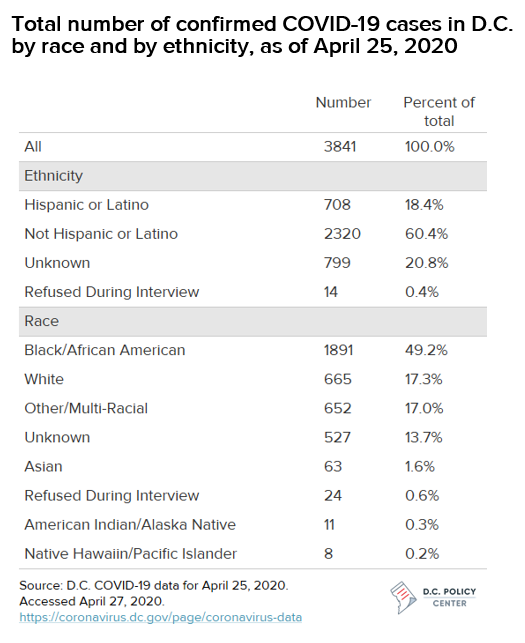
As of April 25, 3,841 District residents have tested positive, and 178 have died as a result of COVID-19. Over 18,000 people in D.C. have been tested overall. While the virus recognizes no geographic boundaries, its impact has varied dramatically across the city. Overall, Ward 8 residents have accounted for the highest share of fatalities in D.C. (41 deaths, or 23 percent of the total), while Ward 2 residents accounted for the fewest (six deaths, or three percent). As of April 25, nine residents experiencing homelessness had died due to COVID-19, representing five percent of COVID-19 deaths in D.C.
In D.C. and across the country, the confluence of inequities in health access, health outcomes, and socioeconomic conditions has also contributed to disproportionate outcomes by race, with particularly poor outcomes for Black residents. Black residents make up 46.4 percent of D.C.’s population, but roughly half (49 percent) of its confirmed COVID-19 cases to date, and the vast majority (80 percent) of its fatalities, according to the most recent COVID-19 data released by the D.C. government.
This article explores which populations in D.C. are particularly at-risk for severe outcomes from COVID-19, and including how these risk factors are distributed across the District’s population by race. However, while this analysis focuses on groups that appear to be most at risk, based on presently available data, no group is immune; there have been severe cases and fatalities within every age group and across race, ethnicity, income, and social group. For the most recent data and official health information about COVID-19 in the D.C. area, visit coronavirus.dc.gov.
Nationally, older age groups have been disproportionately affected by COVID-19, but underlying health conditions present risks across age groups.
While most people with COVID-19 recover without requiring hospitalization, people with at least one serious underlying health condition are more likely to be hospitalized or need an intensive care unit and are at a higher risk of a fatal outcome. According to CDC guidance, serious underlying health conditions and other potential risk factors currently include:
- Chronic lung diseases, such as chronic obstructive pulmonary disease (COPD)
- Diabetes
- Serious heart conditions or cardiovascular diseases
- Chronic kidney disease
- Being immunocompromised[1]
- Severe obesity
- Asthma, and
- Liver disease
Definitions of which groups are potentially more at risk differ slightly across different health groups, and may change as more data is available. According to early estimates released by the Centers for Disease Control and Prevention (CDC), the most commonly reported underlying conditions among patients for whom information was available appear to have been diabetes, chronic lung disease (including COPD, asthma, and emphysema), and cardiovascular disease.
The CDC estimates that 71 percent of patients who are hospitalized (but not admitted to the intensive care unit, or ICU) and 78 percent of those who are admitted to the ICU had at least one of these underlying conditions. Some of these conditions are more likely to result in intensive care – for instance according to CDC’s analysis, 32 percent of ICU patients had diabetes.
Nationally, COVID-19 has so far disproportionately affected older adults, with 80 percent of deaths occurring amongst those aged over 65 years. Part of the reason older adults more at risk appears to be related to overall health: Among D.C. residents over the age of 65 years, for example, 54.7 percent have one or more of four relevant underlying health conditions (e.g., COPD, diabetes, coronary heart disease, obesity), which further compounds the threat of having a severe experience of COVID-19.
As of 2018, the population of those over the age of 65 years was 81,712 in D.C., which comprises 12 percent of the total population. Within this category, 28.8 percent of these older residents were recorded as the only adult living in their household. In terms of race and ethnicity, Black residents make up a greater share of D.C.’s older population compared to its younger population: Among residents age 65 and older, 58.3 percent are Black, 36.8 percent are white, and 5 percent are Hispanic or Latinx. Another 2.4 percent are Asian, 0.5 percent are categorized as American Indian or Alaskan Native, and 2.6 percent are some other race.
However, while underlying health conditions are more common among older adults, the numbers are still significant for younger age groups. For example, among D.C. residents between the ages of 18 and 64 years, 11.9 percent have asthma, 6.3 percent have diabetes, and 6.8 percent have a chronic lung disease or serious heart condition.
Among those with COVID-19, people of color are more likely to experience the most severe outcomes.
National data reported by the New York Times, Washington Post, and others shows that there have been major racial disparities in COVID-19 health outcomes. The disproportionate impact of COVID-19 appears to be connected to a variety of interlocking factors of structural racism that affect who is most likely to be exposed to the virus, who is most at risk of severe outcomes, and who is most likely to die as a result.
These trends are also present in D.C., particularly among Black residents. According to the most recent COVID-19 data released by the D.C. government, Black residents make up 46.4 percent of D.C.’s population, but roughly half (49 percent) of its confirmed COVID-19 cases to date, and the vast majority (80 percent) of its COVID-19 fatalities. Hispanic or Latinx residents are also overrepresented in the number of confirmed cases, accounting for 11.3 percent of D.C.’s population but 18 percent of cases (and 6 percent of deaths).
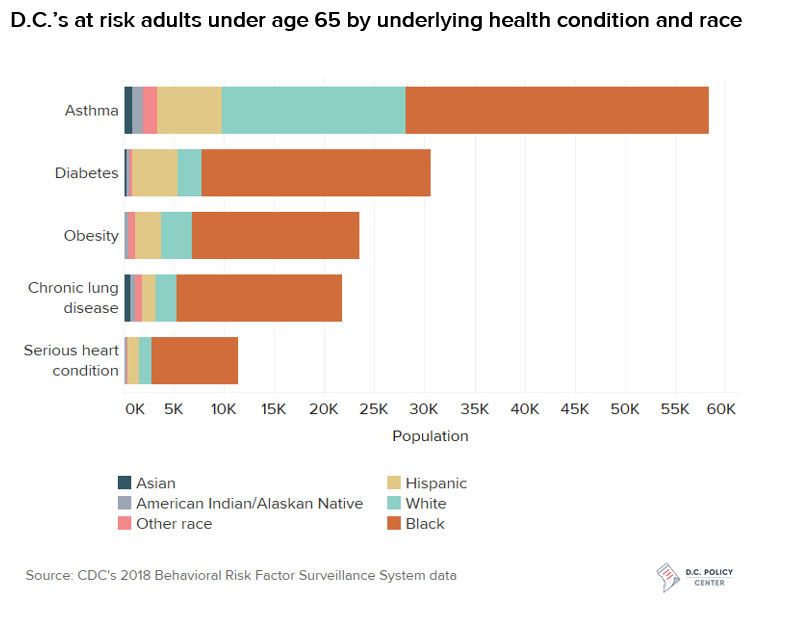
The underlying health disparities are significant, as the District’s Black residents are more likely to be affected by diabetes, obesity, high blood pressure, asthma, lung disease and heart disease. Several of these are shown in the chart below, which shows the number of D.C. residents under the age of 65 with five health conditions that the CDC has cited as at-risk for worse COVID-19 outcomes, broken down by race.
Some groups are also at greater risk of exposure to the coronavirus in the first place
While much of the country is under stay-at-home orders, not all workers can conduct their jobs remotely. An analysis by the New York Times suggests that nationally, higher-income workers were far more likely to be able to work from home: 61.5 percent of workers in the top income quartile are able to work from home, compared with just 9.2 percent of workers in the bottom income quartile.
A recent working paper examining which jobs are most likely to be able to work from home found that 50 percent of workers in the D.C. metropolitan region could potentially work remotely, the second-highest share in the country. However, people of color are disproportionately likely to work in occupations that have high levels of individual contact during the pandemic (or be out of work altogether). In D.C., Black residents make up the vast majority of healthcare support workers (74.1 percent), which includes personal care aides, home health aides and nursing assistants; protective services workers, such as firefighters and police officers (74 percent), and transportation workers (83.7 percent).
Likewise, the Washington Post reports that Prince George’s County, where more than six in ten residents are Black has seen the greatest number of COVID-19 cases in the metropolitan area (4,987) and almost as many deaths as D.C. (174), in large part “because many residents are front-line workers exposed daily to the virus, and Prince Georgians disproportionately suffer from underlying health conditions that make the virus more deadly.” Black residents currently account for almost 70 percent of the county’s COVID-19 fatalities.
Many groups are also at higher risk of exposure to the coronavirus due to the relatively crowded nature of their living conditions, among other factors. For instance, people living in nursing homes or long-term care facilities are also at higher risk, due both to their living conditions and to the higher prevalence of underlying health conditions. In D.C., there have been 141 cases at long-term care facilities, and 14 resident deaths.
People who are incarcerated are also at high risk: In the District, people in custody of D.C.’s Department of Corrections (DOC) have experienced an infection rate 15 times that of the District as a whole. As of April 25, 125 residents in the custody of the Department of Corrections had tested positive for COVID-19, and one had died; one DOC worker has also died, and 37 have tested positive. A U.S. District Judge recently ordered the D.C. Jail to address serious health and sanitation concerns in the Jail in response to a class-action lawsuit filed by the American Civil Liberties Union of DC and the Public Defender Service for the District of Columbia.
* * *
While the impacts of COVID-19 have been sudden, the racial inequities it has deepened in D.C. and elsewhere have been generations in the making. Likewise, while the District will work to stem the worst effects of the pandemic in the weeks and month ahead, its work to rebuild its hardest-hit communities will take years and concerted effort across many sectors.
To read more about the impact of COVID-19 in the District of Columbia, click here.
About the data
This analysis defines D.C.’s high-risk population as those over 65 years of age and adults with cardiovascular (heart related) disease, chronic obstructive pulmonary disease (COPD; lung related), asthma, or cancer (immunocompromised). Health estimates were calculated using CDC’s 2018 Behavioral Risk Factor Surveillance System (BRFSS), which is an annual telephone survey that collects state data about civilian health-related risk behaviors, chronic health conditions, and use of preventive services. The census tract level data was obtained through the CDC’s 500 Cities: Local Data for Better Health (2019 release) which included 2017 BRFSS data based small area estimates for chronic diseases.
Age and race/ethnicity based population counts were calculated using the U.S. Census Bureau’s 2014-2018 American Community Survey 5-Year estimates.
Occupation data by race is based on the U.S. Census Bureau’s 2018 American Community Survey 1-year Estimates (S2401).
Notes
[1] Including “including cancer treatment, bone marrow or organ transplantation, immune deficiencies, HIV with a low CD4 cell count or not on HIV treatment, and prolonged use of corticosteroids and other immune weakening medications.”
Sunaina Kathpalia is a Research Assistant at the D.C. Policy Center.
Kathryn Zickuhr is the Director of Policy at the D.C. Policy Center.