America’s drug problem continues to evolve in startling and dangerous ways, and the District of Columbia remains at the forefront of those changes. Drug overdose continues to be a leading cause of death in the United States; according to the latest figures from the Centers for Disease Control, the national death toll from drug overdose reached 72,000 in 2017. But those numbers fail to capture some of the most alarming new developments—among them, synthetic drugs.
Inexpensive, easily manufactured drugs like fentanyl and synthetic cannabinoids represent a new chapter in the drug crisis. Fentanyl is already a major driver of mortality in the opioid epidemic, both in D.C. and nationwide, and repeated outbreaks of synthetic cannabinoid poisonings have troubled cities across the nation. A pair of mass overdose events in D.C. and New Haven, Connecticut drew national attention in July, and the entire Pennsylvania prison system went into lockdown in early September over fear of widespread exposure. Another outbreak struck the District last month as rescue crews evaluated over 100 people within a three-day period. D.C. authorities are currently investigating five deaths related to that outbreak.
Even amidst positive signs—including a noticeable slowdown in regional opioid deaths[1] and incremental progress on the public health front—cities like D.C. are increasingly vulnerable to the changes wrought by synthetics. Over the last several years, synthetics have made such deep inroads into U.S. drug supplies that any contamination or sudden shifts in potency can have deadly consequences for a city or an entire region.
Those consequences are further exacerbated by the federal government’s insistence on a strategy of prohibition, which encourages traffickers to move toward more powerful and easily smuggled drugs and increases the challenge to medical providers and first responders. Addressing the drug crises of today—and tomorrow—requires a new approach to drug policy, one that seeks to reduce harm to users instead of incarcerating them.
The fentanyl epidemic
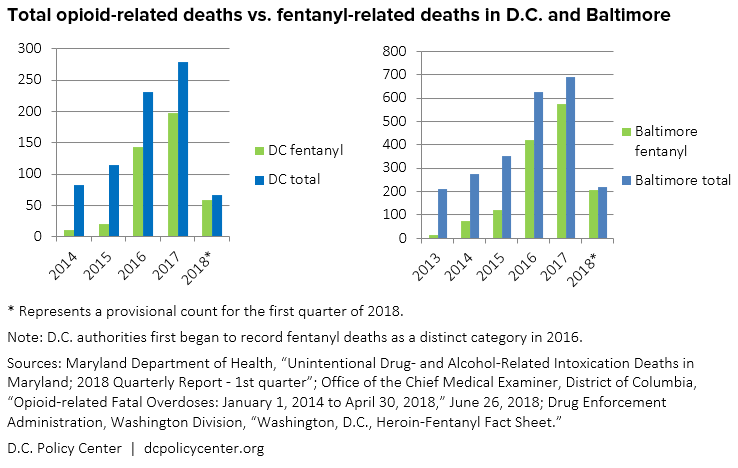
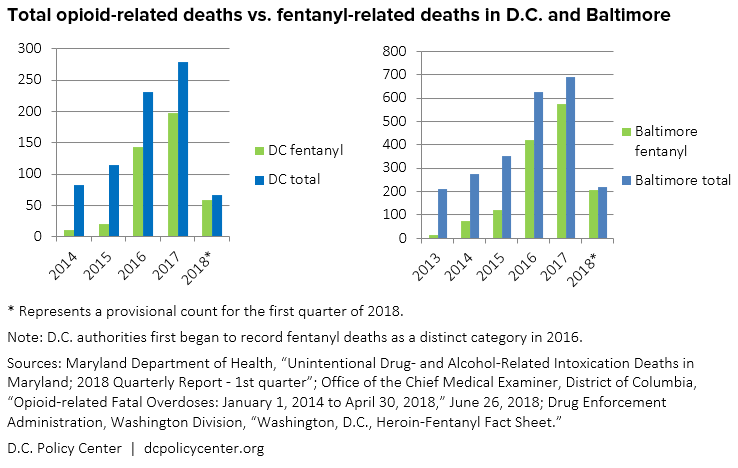
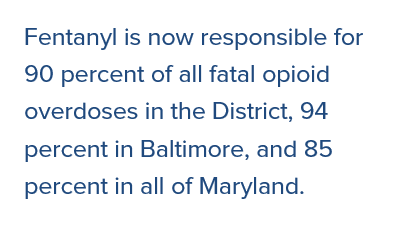
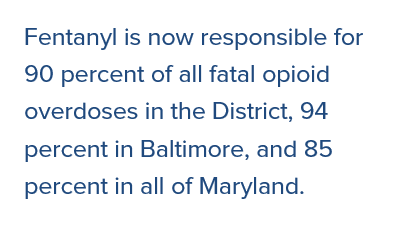
In terms of total fatalities, the most notorious of synthetic drugs remains fentanyl and its derivatives, which are believed to be responsible for about half of all U.S. opioid deaths in 2017. The District, along with other cities of the East Coast and Midwest, has been on the leading edge of this increasingly fatal turn. As the D.C. Policy Center previously reported, fentanyl first began to make a substantive impact on local overdose rates in 2015, and drove a dramatic spike in 2016. Local health agencies estimate that fentanyl is now responsible for 90 percent of all fatal opioid overdoses in the District, along with 94 percent in Baltimore and 85 percent in all of Maryland.
Roughly 50 to 100 times more powerful than morphine, fentanyl has had an important place in American medicine for decades because the strength and speed at which it works makes it extremely effective at short-term pain relief. But fentanyl stands apart from other narcotics for more than just its potency.
Unlike morphine, heroin, or many prescription opioids, whose neurochemical properties ultimately derive from the opium poppy, fentanyl is purely synthetic and created entirely in the laboratory, making it relatively easy and inexpensive to produce. This affects more than the price. By removing drug manufacture from any basis in agriculture, synthetics disrupt the longstanding political, economic, and criminal relationships that traditionally underpin international drug flows and make it more difficult for governments to assert control. That difficulty flows downstream to police operating at the global level and on the street, while traffickers gain a low-cost product that simultaneously strengthens and stretches heroin supplies. The result is fentanyl’s almost total saturation of illicit markets throughout the region.
Fentanyl’s unpredictable potency in unregulated street drugs has also created an active mythology that undermines public health and policy responses. Contrary to sensational media portrayals and police reports, fentanyl cannot be absorbed through the skin, and the risk of exposure through airborne particles is minimal.
Comparing the alarm over fentanyl exposure to the panic over contagion during the AIDS crisis, University of Pittsburgh medical toxicologist and emergency physician Dr. Ryan Marino says, “this new fear that any symptom in proximity to drugs or drug users can be attributed to fentanyl has led to a snowballing of unsubstantiated reports over the past few years,” and is particularly damaging if it delays emergency response or resuscitation. On social media, Marino and other public health advocates have begun to label such reporting with the hashtag #WTFentanyl. Concern is appropriate, they point out, but panic is not.[2]
In an apparent effort to correct some of these misconceptions, the White House Office of National Drug Control Policy recently released a list of safety precautions for police and first responders, together with a highly stylized training video that offers, at best, a mixed message about the dangers and realities of fentanyl exposure.
According to the Drug Enforcement Administration[3], most of the fentanyl on American streets comes from China by way of Mexico and enters illicit supplies at the wholesale level. Today, fentanyl is most commonly found in the powdered heroin prevalent in the Mid-West and eastern United States. But it’s also begun to show up around the rest of the country and in a variety of other forms as well: pressed into counterfeit pills, mixed with black-tar heroin, and in combination with an assortment of other drugs like cocaine and methamphetamine—as well as synthetic cannabinoids.
The synthetic revolution
Man-made lab-born drugs like fentanyl aren’t new. Amphetamines were synthesized in the late nineteenth century and further developed in the early twentieth century, along with other drugs like MDMA, PCP, and cathinones (aka bath salts, which mimic and amplify the stimulant effects of the khat plant). Fentanyl was created in the 1960s, and each of these drugs has provoked periodic crises in the years since. What has changed is the speed at which new and ever more powerful synthetic drugs are reaching unprepared users.
In Forces of Habit, historian David Courtwright describes a phenomenon he labels the psychoactive revolution, whereby “people everywhere have acquired progressively more, and more potent, means of altering their ordinary waking consciousness.” Synthetic drugs and modern chemistry have sped that process beyond society’s ability to evolve social and cultural mechanisms that promote safe drug use, or to create legal structures capable of controlling the most volatile substances.
“Synthetic cannabinoids, synthetic opioids, or synthetic cathinones—all of these can be manipulated fairly easily and fairly cheaply, and it just depends upon what is currently the new next best thing,” says Dr. Luke Short, Manager of the Chemistry Section and Forensic Chemistry Unit at D.C.’s Department of Forensic Sciences. “Next year could be something very different.”
Fentanyl has spawned a host of analogs and derivatives, including carfentanil, which is roughly 100,000 times more powerful than morphine. Last year, D.C. officials detected an entirely new, previously unreported variant called methoxyacetyl fentanyl. The challenge to local authorities is that, with just a few minor tweaks to their chemical structures, these drugs evolve and iterate faster than they can be detected, controlled, or outlawed—a broader problem starkly illustrated by these recurring outbreaks of synthetic cannabinoid overdoses.
Synthetic cannabinoids
The first thing to know about synthetic cannabinoids, sometimes called synthetic marijuana or fake weed, is that they are not, in fact, anything like marijuana. This misnomer is more than a technical point; it associates a relatively safe drug with a class of incredibly dangerous drugs, and that can have lethal consequences for unsuspecting users.
- Synthetic cannabinoids as dried plant material
- Examples of synthetic cannabinoids packaging
Examples of synthetic cannabinoids, courtesy of the D.C. Department of Health. While K2 and Spice were some of the earliest brand names for synthetic cannabinoids, more recent names include Scooby Snax, Bizarro, Mr. Nice Guy, and Red Dawn X. (Source: D.C. Department of Health, Synthetic Marijuana Can Be Deadly.)
Synthetic cannabinoids are actually an ever-changing potpourri of chemicals (sometimes literally sprayed on potpourri) designed to act upon the brain’s cannabinoid system—the same bundle of receptors activated by tetrahydrocannabinol (THC), the main psychoactive ingredient in actual marijuana. But that’s about where the similarities end, as the physiological effects of synthetic cannabinoids are quite different and unpredictable. Making matters worse, synthetic cannabinoids are frequently mixed with other drugs, like cathinones, fentanyl, and even rat poison. The resulting cocktail produces an array of dizzying symptoms, including elevated and irregular heart rate, nausea, severe agitation, hallucinations, confusion, seizures, and psychosis, as well as serious second order effects like heart attack, kidney failure, and stroke.
Dr. Jenifer Smith, Director of the District’s Department of Forensic Sciences, describes synthetic cannabinoids as “the Russian Roulette of chemistry—you don’t really know what you’re ingesting.” One of the problems, she says, is that “there are no metabolic studies. Because these are not legitimate pharmaceuticals, you can’t really subject people to testing,” and that means “we don’t actually know what it is going to do to you—other than they are all pretty nasty.”
Despite their wildly different effects, synthetic cannabinoids are marketed as an inexpensive and readily available alternative to marijuana. Branded with names like Spice, K2, and Scooby Snax, synthetic cannabinoids first appeared in the early 2000s, often as a mix of ground-up plant matter sprayed with chemicals to approximate the appearance of marijuana. Sold by both convenience stores and street dealers, they exist in a regulatory grey zone as new blends and compositions stay one step ahead of legal controls.
D.C. was first troubled by a major outbreak of synthetic cannabinoid poisonings in the summer of 2015, and the drug has resurfaced in periodic episodes ever since. The danger was dramatically underscored this July, when D.C. saw over 300 overdoses within a single two-week period. DCist reports that over 200 people were hospitalized, and the Washington Post reports that emergency response crews evaluated 785 individual cases by the end of August. At least five more people died in another spike of overdoses earlier this month.
These outbreaks put a strain on city services, including police and emergency medical crews. Kevin Donahue, Deputy Mayor for Public Safety and Justice, says, “The recent spike in overdoses has had a significant impact on the availability of EMS staff and apparatus, which are in demand throughout the city for all emergency medical needs.”
Dr. Smith’s lab was able to confirm that the latest batch to rock the city does not contain rat poison, as has been reported in other cities, nor does it yet appear to contain fentanyl. Nevertheless, Dr. Smith emphasizes, “This stuff is dangerous.” For now, the current supply consists of the usual base chemicals, plus some new additives—none of which are found in nature. “It looks like the drug dealers are just playing with different other ‘spices’ that they are adding into it now and then,” explains Dr. Short.
These clusters of cannabinoid poisonings are not confined to D.C. Within the last few years, similar outbreaks have been reported in big cities across the nation, including Baltimore, Brooklyn, St. Louis, Dallas, Austin, LA, and New Haven, where more than 90 people fell victim in a single mass overdose event in a public square in August. The common denominator in each is the convergence of synthetic cannabinoids with low-income and homeless populations, layering a dangerously volatile drug atop a host of pre-existing socioeconomic and health challenges.
At first glance, this latest outbreak is even more perplexing here in the District, where marijuana has been legal since 2015. But in the context of the synthetic revolution and America’s larger troubled relationship with drugs, the growing problem of synthetic cannabinoids is hardly surprising. These episodes are ultimately the consequence of a stratified drug market.
The divided marijuana market
Despite legalization, not everyone in D.C. has access to legal marijuana. Congressional obstruction has prevented D.C. from establishing any kind of dedicated marijuana retail outlets, forcing sales into a grey market and “gift” economy—and keeping a relatively safe drug more scarce and expensive than it otherwise would be in a fully licit market. Synthetic cannabinoids, on the other hand, are inexpensive and easily accessible, with individual doses going for as little as $2, and smaller packets around $10. “These [synthetic] drugs are so cheap that it’s very difficult to prevent people from taking them, except through trying to educate as best we can,” says Dr. Smith.
![“These [synthetic] drugs are so cheap that it’s very difficult to prevent people from taking them”](https://www.dcpolicycenter.org/wp-content/uploads/2018/10/pullquote2.png)
![“These [synthetic] drugs are so cheap that it’s very difficult to prevent people from taking them”](https://www.dcpolicycenter.org/wp-content/uploads/2018/10/pullquote2.png)
The fact that marijuana is still not legal at the federal level also drives demand for synthetic “alternatives.” Sanho Tree, a drug policy expert at the Institute for Policy Studies, explains that synthetic cannabinoids tend to be “a substitute drug of last resort,” marketed to homeless populations “who can’t afford other types of drugs, and near military bases, where soldiers believe the synthetics wouldn’t show up in regular urine tests.”
The consequences of this divided market are analogous to the harm caused by wood alcohol during Prohibition. With legal production and sites of consumption outlawed, alcohol went underground, and quality and safety suffered. Wealthy elites continued to enjoy access to high-quality hooch and enjoyed the newly transgressive allure of defying the law; meanwhile, the poor and working class experienced aggressive policing and were left with a highly adulterated and dangerous product that produced an array of negative health outcomes, like blindness, paralysis, and death.
The popular consensus on the lessons of Prohibition (and its repeal) is that America realized the futility of legislating private behavior, recognizing that prohibition merely drove drug markets and consumption into the dark where actual control proved impossible. As a society, we may have made our peace with alcohol, but the full implications of these lessons have yet to sink in.
The solutions: Decriminalization, regulation, and beyond
The lessons of the past suggest that simply banning drugs—even very powerful drugs—will continue to have harmful effects on public health. D.C. has tried and failed to outlaw synthetic cannabinoids for years, and is now moving to increase penalties on vendors. Drugs that are so obviously harmful to human health and society do require some form of control, but the prohibitionist approach is clearly an uphill battle.
In the end, synthetic drugs like fentanyl and cannabinoids will pose a threat so long as drug markets remain so sharply stratified and illicit supplies or grey market products remain easier to access than treatment or comparatively safer alternatives.
This fact underscores the need for regulation. The growing number of outbreaks involving synthetic cannabinoids illustrates how the problem of unregulated illicit supplies goes beyond heroin and fentanyl. It’s no secret that drug supplies are increasingly dangerous, but that’s not necessarily a sufficient deterrent to use.
There are steps local officials can take to reduce the immediate harm, starting with addressing why people seek out these dangerous drugs in the first place: cost and access. District citizens and policymakers should renew the push for legal marijuana retail, which should improve access and reduce the appeal of synthetic alternatives. To reduce harm to low-income communities, Sanho Tree of the Institute for Policy Studies even suggests allowing volunteers to grow and distribute free marijuana near homeless shelters. “Nobody should be driven toward these high-risk synthetics because of poverty,” says Tree.
Further decriminalizing public use is another important tactic. In just the last few days, Mayor Muriel Bowser and Metropolitan Police Department Chief Peter Newsome took a step in the right direction by announcing that police would issue a $25 fine for public consumption of marijuana instead of making an arrest. Deputy Mayor Donahue says the city has also begun to forward deploy paramedics and public health officers who “go out proactively on a daily basis at known spots with a heavy concentration of usage.”
In the big picture, it’s also time for D.C. to revisit conversations around forward-looking harm reduction techniques like drug checking and safe consumption sites. San Francisco, Seattle, New York, and Philadelphia are all taking a hard look at the feasibility of supervised injection facilities like that pioneered by Vancouver. Although the politics are contentious, the science is strong,[4] and such facilities are a critical tool for public health teams to reach vulnerable populations—precisely those that were hardest hit by the recent spate of cannabinoid poisonings. The overdose crisis goes beyond opioids, and D.C. has an opportunity to help lead the national response.
One of Mayor Bowser’s most important and overlooked initiatives has been to improve the city’s capacity to monitor the illicit drug supply. Until recently, the DEA was responsible for conducting lab work on drugs seized in the city, typically in support of criminal prosecution. But D.C’s Department of Forensic Sciences steadily built a strong surveillance capacity to monitor the chemical make-up of local drug supplies after the 2015 spike in cannabinoid poisonings. With Mayor Bower’s support, the city opened a dedicated drug lab in April of this year. This, too, is a step in the right direction. “We hope we can add good information,” Dr. Smith says. “We’re pretty excited about being able to take a broader approach so we have a better understanding of what might be in the drug supply.”
Monitoring local drug supplies is an important public health service that can help cities better respond to the sudden crises unleashed by synthetics, and in time it can provide the foundation for the kind of drug checking capacity that can help prevent needless overdose deaths.
In some quarters of American culture, drug checking and safe consumption represent a moral compromise. But the goal of a drug-free America isn’t realistic—and it ignores the harm done by legal drugs. Alcohol, according to a new study in The Lancet, is estimated to kill nearly 3 million people a year worldwide and about 90,000 in the United States. In Maryland, the number of people killed by acute alcohol intoxication jumped from 310 in 2015 to 582 in 2016. And despite decades of declining cigarette use, tobacco remains the most lethal drug of all, responsible for the death of nearly half a million Americans every year—a number that should give pause as the surging popularity of vaping and e-cigarettes continues to outstrip regulation or knowledge of their health risk.
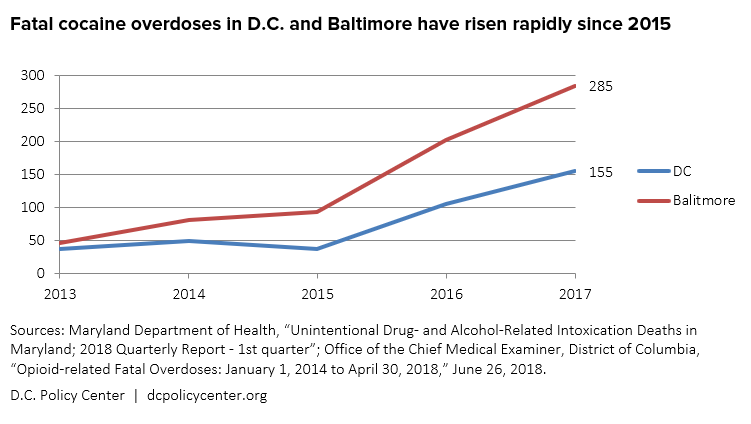
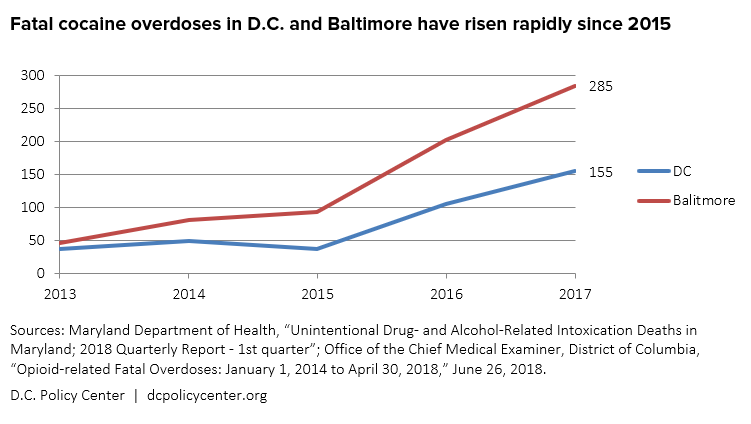
Meanwhile, the understandable focus on opioids overshadows the growing toll of other drugs of abuse, like legally prescribed benzodiazepines and a serious spike in cocaine use. Baltimore, for example, saw a 200 percent increase in fatal cocaine overdose between 2015 and 2017.
Immediate concerns like the rise of synthetic cannabinoids and the opioid epidemic are symptomatic of a larger social problem, merely the latest and most damaging episodes in America’s troubled relationship with drugs, both legal and illegal. And we can’t address these emerging dangers—or broader trends like the rise of synthetics—in isolation from America’s overall drug crisis. The acute rise in overdose deaths demands both immediate policy responses and a deeper cultural reckoning. It’s time to rethink our social and political response to the harm caused by all drugs, regardless of legality—a status that more often reflects racial and socioeconomic tensions than actual pharmacology and impedes the public health strategies necessary to turn the tide.
Data sources
Chart: Total opioid-related deaths vs. fentanyl-related deaths in D.C. and Baltimore
- Maryland Department of Health, “Unintentional Drug- and Alcohol-Related Intoxication Deaths in Maryland; 2018 Quarterly Report – 1st quarter.”
- Office of the Chief Medical Examiner, District of Columbia, “Opioid-related Fatal Overdoses: January 1, 2014 to April 30, 2018,” June 26, 2018.
- Drug Enforcement Administration, Washington Division, “Washington, D.C., Heroin-Fentanyl Fact Sheet” (PDF)
Chart: “Fatal cocaine overdoses in D.C. and Baltimore have risen rapidly since 2015”
- Maryland Department of Health, “Unintentional Drug- and Alcohol-Related Intoxication Deaths in Maryland; 2018 Quarterly Report – 1st quarter.”
- Office of the Chief Medical Examiner, District of Columbia, “Opioid-related Fatal Overdoses: January 1, 2014 to April 30, 2018,” June 26, 2018.
Notes
[1] In 2016, the number of fatal overdoses in the District doubled over the previous year, but the most recent report from D.C.’s Office of the Chief Medical Examiner indicates that the rate of fatal overdose increased by only 21% in 2017. Maryland’s rate of increase slowed from 70% to 8% over the course of 2017, and Baltimore’s rate of increase slowed from 77% to 10% over the same period. Nationwide, the number of new heroin users is estimated to have dropped by about half.
[2] One of the most illustrative examples of this level of panic occurred in late August at Ross Correctional Institute in Chillicothe, Ohio, in an incident where 27 prison staff members were apparently sickened and reported nonspecific symptoms after exposure to a substance later confirmed as a mixture of heroin and fentanyl. Multiple individuals were treated with naloxone (a medication that reverses an opioid overdose), but only one individual was admitted to the hospital.
[3] See in particular pages 57-66.
[4] A recent much-publicized study challenging the efficacy of safe injection sites was recently retracted due to poor methodology.
Matthew R. Pembleton is the author of Containing Addiction: The Federal Bureau of Narcotics and the Origins of America’s Global Drug War (UMass Press, 2017) and teaches at American University. He is also a history consultant at the National Academies of Sciences, Engineering, and Medicine. Follow him on Twitter at @mattpembleton.


